Experiences with nutritional follow-up and barriers and opportunities of implementing digital seamless nutrition care in the head and neck cancer treatment course: a qualitative study from patient, family caregiver, and healthcare professional perspectives | BMC Health Services Research

A total of seven patients, four spouses, five registered nurses (three from an outpatient clinic and two from a hospital ward), and two physicians participated in individual interviews. The included patients, of whom five were male, all had a HNC diagnosis. Six of the patients were married and six had a college or university degree. The patients’ age ranged from 59 to 79 years, with a mean of 66 years. Three of the spouses were female. with ages ranging from 55 to 68 years, and a mean age of 61 years. Of the HCPs, six were female, and the mean age was 42 years, with a range from 29 to 60 years. The HCPs had experience from working with HNC patients ranging from 4 months to 25 years, with a mean of 9.8 years.
Overview
The results are presented according to the two aims of the study. First, we explored the experiences of patients and spouses with the nutritional follow-up throughout the HNC treatment course, which resulted in three themes. Second, we identified potential barriers and opportunities with the NUTREAT intervention from the perspectives of key stakeholders, resulting in four themes corresponding to four of the domains in the updated CFIR. Figure 2 provides an overview of these experiences, as well as the identified barriers and opportunities associated with the planned NUTREAT intervention.
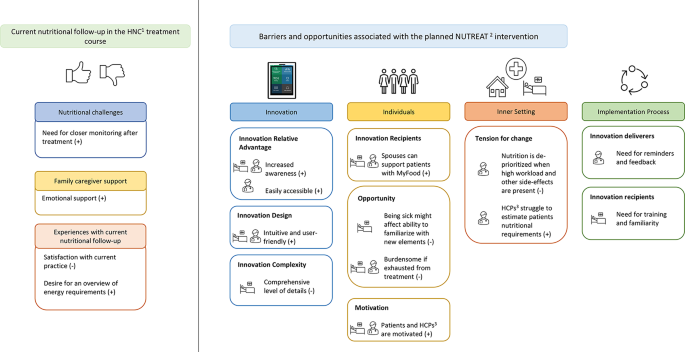
Experiences with nutritional follow-up and identified barriers and opportunities associated with the planned NUTREAT intervention. Themes are presented in bright colors, and sub-themes in bold. The first column corresponds to findings regarding experiences with current nutritional follow-up. The last four columns correspond to domains of the updated consolidated framework for implementation research [32]. + indicates potential opportunities. – indicates potential barriers. Implementation process indicates prerequisites for the upcoming effect and implementation study. The symbols represent the different respondents reporting on the various topics. 1HNC: Head and neck cancer; 2NUTREAT: Nutrition Throughout the Treatment Course; 3HCPs: Healthcare Professionals
Current nutritional follow-up in the HNC treatment course
Three themes were created based on interviews with patients and spouses regarding their experiences with the current nutritional follow-up throughout the treatment course: [1] Nutritional challenges [2], Family caregiver support, and [3] Experiences with current nutritional follow-up (Fig. 2).
Nutritional challenges
All patients reported varying degrees of nutritional challenges throughout the treatment course, and all patients experienced treatment side effects that affected dietary intake, thereby leading to weight loss. The most reported nutrition-related symptoms were mouth dryness, sore throat, and alterations in taste, and the patients reported that symptoms occurred by the second or third week of treatment and worsened towards the end of treatment and the first weeks after treatment completion. One patient was admitted to the hospital ward during the treatment period, and another was admitted after completing treatment due to insufficient nutritional intake and need for enteral nutrition.
Some patients reported that they lost more weight in the period after completion of radiotherapy, and related this to lack of follow-up in the period following the end of treatment:
And the last kilo and a half, or almost two kilos, I actually lost afterwards [after completion of radiotherapy]. Because then I relaxed a little too much. It was still painful, and then there was no one pushing me all the time. So, I got on the scale at the pharmacy. And then I realized that ‘now you have to’, then I started to eat a little again, and then I thought that now I can eat, now I can drop these stupid nutritional drinks, but I couldn’t. (Patient 7)
Family caregiver support
Most of the patients reported receiving support and encouragement from their spouses for maintaining an adequate dietary intake. They were generally satisfied with the degree of their spouse’s involvement in their nutritional situation and experienced being met with understanding if they could not bear to eat. However, some patients were highly encouraged to increase their food intake by their spouses, and experienced towards the end of treatment that caregivers resigned and did not want to push more on food intake:
My spouse got tired of me saying no thank you. Then they said ‘you can handle this yourself. I can’t be your nanny now, now you have to manage. But you know it’s in the fridge, in the freezer’. It’s still there. (Patient 5)
Some of the spouses described that their most important role was to act as emotional support for the patient, in addition to supporting the patient to make the treatment course smoother. However, the degree to which the spouses were involved in the treatment course, varied. Some spouses attended all the hospital appointments and most treatments, whereas others attended only a few. Some spouses also expressed feeling that they had to push the patient a lot to get them to eat:
So, I was always asking them, ‘have you eaten today?’ and ‘what have you eaten?’. And if they meant that they didn’t want to, that they hadn’t eaten that much, then they had to top up with these nutritional drinks that they had received at the pharmacy. (Spouse 4)
Experiences with current nutritional follow-up
Both patients and spouses reported that they were mostly satisfied with the nutritional follow-up from the hospital throughout the treatment course:
I think it’s been very good. Good follow-up… all the way through basically. (Patient 3)
However, some patients and spouses expressed that they did not feel cared for by HCPs, and one patient had a particularly critical comment:
They have no thought for you, it’s just their profession they’re interested in somehow. The patient is merely a necessary evil. (Patient 5)
Both patients and spouses reported that HCPs emphasized nutrition and maintaining a satisfactory nutritional status throughout the treatment course, especially at the beginning of treatment. Most of the patients were particularly satisfied with the first consultation with the registered dietitian. However, some reported that they became more fatigued later in the treatment course, and that they were unable to absorb the information they were provided. Furthermore, some patients experienced that they received helpful information, but that they were unable to make use of it:
We had a long conversation with the dietitian, which my spouse took part in. It was more than enough, we got ideas about everything possible, both good things to drink and eat. And suggestions for good food. But it didn’t help. When the head doesn’t want to eat. (Patient 5)
Moreover, one spouse reported that they had contacted the hospital on several occasions and were satisfied with the response they received each time. In contrast, another spouse reported difficulties in knowing whom to contact, and that their attempts to reach the hospital often failed:
That you didn’t have one physician, nor one nurse. So, what I strongly urge, is that people who are going through this process, they have an enormous need to have one contact person. One coordinator, to whom you can turn. Because, things come up, i.e., suddenly there is no more eating normally, you have to switch to something else. And getting hold of people on the phone is a huge problem. You get 30 such business cards from the hospital. None of them were ever available. So, it was a bit like, random, if you met someone. And if you met someone, it was someone who didn’t know anything, who would try to call you back. (Spouse 1).
Upon completion of the treatment course, most patients did not receive any additional nutritional follow-up from HCPs at the hospital or their general practitioner. Although most patients and spouses reported being encouraged by HCPs to seek further follow-up if needed, they did not do so neither during nor after treatment completion. Some patients were, however, followed-up by a district dietitian or a cancer coordinator after treatment completion and were satisfied that they were not left to manage on their own. Two of the patients also reported a desire to receive a daily or weekly menu for inspiration on what to eat and get an overview of the number of calories they need to fulfill their requirements.
Identified barriers and opportunities using the updated consolidated framework for implementation research
In the following, identified barriers and opportunities to implement the NUTREAT intervention into the treatment course for patients with HNC are presented according to the five domains of the updated CFIR framework [32] and further sorted into relevant constructs and subconstructs. Four themes, and 25 sub-themes were created, covering a total of 4 domains, 20 constructs, and 5 subconstructs as illustrated in Supplementary file 4. The constructs are highlighted in brackets in the result descriptions.
Innovation domain
Innovation entails the NUTREAT intervention, with the MyFood app as a central component. The proposed plan for the NUTREAT intervention involves patients receiving the intervention and HCPs using information from the MyFood app in the electronic patient record to support their workflow and provide additional nutritional follow-up if needed.
HCPs and spouses unanimously agreed that a good nutritional status plays a major role in treatment and recovery, in addition to contributing to less pronounced side effects and greater tolerance of the treatment (Innovation evidence base):
If the patient gets the nutrition they should have, then they complete the treatment much better. They are stronger and the side effects are not as pronounced as when they are malnourished or do not eat or drink. Then it kind of gets worse. Everything gets much worse. So, I think that nutrition has a lot to say. (Nurse 1).
The MyFood app was considered intuitive and user friendly by most of the participants. The layout was perceived as satisfactory as it does not require the entry of free-text input (Innovation design). However, one patient raised concern towards the level of details required in the dietary recordings, suggesting that it might be too comprehensive, time consuming, and easy to forget (Innovation complexity):
It looks simple, but it is a bit extensive. It may not take long, but… detailed, yes. (Patient 2)
MyFood was considered more accessible than the current paper-based dietary recording forms and was believed to contribute to earlier detection of nutritional problems than the current practices. Providing objective measures of patients’ nutritional status and increasing patient awareness of nutritional requirements were considered benefits of the NUTREAT intervention. Additionally, it was stated that the NUTREAT intervention could save time and increase focus on nutrition among HCPs (Innovation relative advantage):
I think the most important benefit of it [the intervention] is that those who are to give the patient advice have the information already before meeting the patient. (Patient 7)
Furthermore, one spouse emphasized the importance of HCPs following up on the recorded intake. They expressed concern that patients might lose interest of using the MyFood app if they do not experience that the recorded intake is being monitored by anyone:
I think it can make the treatment better if it’s followed up. That there is someone monitoring it. That it doesn’t just become an instrument you have to use that is not used for anything. So, there must be someone sitting there and following it up. (Spouse 2)
One of the registered nurses suggested that the NUTREAT intervention should be introduced to the patients a few weeks after starting their treatment to optimize the implementation to the HNC treatment course (Innovation adaptability).
Individuals domain
The patients were described by HCPs as a highly diverse group, ranging from resourceful individuals to those struggling with drug and alcohol dependence, spanning varying ages and levels of social support.
Both patients, spouses, and HCPs considered the registered dietitians as important innovation recipients, given their ability to act on the information obtained from the dietary recordings in the MyFood app. Furthermore, all participants considered family caregivers as an important support and resource in assisting the patient with monitoring their dietary intake (Innovation Recipients):
Yes, a caregiver. Because then, if they download [the MyFood app] on their own [device], they can probably go home and help their father or mother or whomever to do it. I believe that a lot of people have very many relatives, who are in a situation where they wish to provide care. And often they don’t know what to do. (Patient 1)
Most patients believed that they would be able to use the MyFood app for dietary recordings, and both patients, spouses, and HCPs assumed that most people today have sufficient knowledge of digital surfaces to be able to use smartphone applications (Characteristics subdomain: Capability). Furthermore, most of the participants, both HCPs, spouses, and patients were positive about the ability of most patients to use the MyFood app for dietary recording. However, some registered nurses and patients were concerned that the intervention might be experienced as burdensome for some, especially for those who are exhausted from treatment, uninterested, elderly, have dementia, or are less resourceful. It was also mentioned that being sick might reduce the ability to familiarize with new elements (Characteristics subdomain: Opportunity):
I can manage an app, I was about to say. I would have managed that app of yours, but at the same time when you are in the illness phase, you are not that interested in a lot of other things in a way, and… Don’t have excess energy to learn new things perhaps. (Patient 1)
HCPs considered the registered nurses at the outpatient clinic implementation facilitators due to their degree of involvement in the study and with the patients. It was stated that the registered nurses could provide assistance to the patients if they should have any questions or challenges regarding the intervention (Implementation facilitators).
In terms of leadership, HCPs expressed that the high-level leaders are little involved in managing the day-to-day operations of each department. They also experienced that these leaders do not monitor whether guidelines for nutritional follow-up for HCPs are being followed. Furthermore, HCPs expressed that they have limited relation to the high-level leaders (High-level leaders):
The head of the department is very present, so it’s not that, but somehow above that [leadership at a higher level] I feel it’s such an informal matter that I don’t really have any particular relationship to. (Physician 2)
HCPs further expressed that they feel it is unclear who their immediate leader is, and that they are mostly in charge of organizing their daily operations themselves. However, it was mentioned by several of the HCPs that the involvement and engagement of the head of the department is considered an important facilitator for implementing new practices, in addition to reminders from their closest leaders (Mid-level leaders).
All the HCPs expressed that they were motivated to be involved in the NUTREAT intervention. Patients and spouses also expressed that they would have been motivated to participate in the intervention if given the possibility. However, some prerequisites were mentioned by some patients for maintaining motivation over time, including being presented with a rationale for why the intervention is important. Some participants also mentioned that the motivation might decrease if the intervention becomes burdensome or if becoming fatigued from the treatment (Characteristics subdomain: Motivation). Another important aspect highlighted by several HCPs was that project group members must be available to answer questions or to solve potential problems to increase the likelihood of successful implementation (Implementation team members):
I think you guys [the project team] must be available if there’s anything we’re wondering about. And that you have clear guidelines for how it should work, or what to do, and follow up, really. (Registered nurse 4)
Inner setting domain
Most HCPs and spouses indicated that they aim to provide patients with the best possible treatment and ensure satisfactory nutritional status. Several HCPs experienced that there are clear hospital guidelines and templates for what to include in the nutritional follow-up of patients. Furthermore, they stated that there are routines for nutritional monitoring of patients at risk of malnutrition. However, there was some discrepancy between what was reported in the interviews by the various HCPs regarding the extent to which they focus on nutrition. Physicians reported that HCPs, in general, are mostly concerned with their specific professional areas, which may lead to poorer nutritional follow-up before the first consultation with the registered dietitian (Communications). One registered nurse related this to the physicians considering nutrition as less important as other aspects of the treatment (Culture):
Or it’s the physician who doesn’t always think it… not as important, but there’s a lot that comes into play there. It could be other issues that are perhaps more important. (Registered nurse 4)
Among the registered nurses at the hospital ward, it was unclear whether they have a designated nutrition resource person, and they expressed that they often tend to leave the responsibility of the nutritional treatment to the registered dietitians because they have several other tasks to attend (Work infrastructure). HCPs also reported a lack of training focused on the nutritional treatment of patients and expressed a desire for more training in this area. However, one registered nurse mentioned that in cases where such training had been offered, the outcomes had been limited (Learning-centeredness).
Both the registered nurses at the hospital ward and the physicians agreed that they experienced close collaboration with the registered dietitians. However, registered nurses at the outpatient clinic experienced that outpatients are not monitored as closely as inpatients in terms of nutrition. They reported experiencing a great distance and little contact with the registered dietitians, and they expressed a desire for closer collaboration (Relational connections):
But I do have a desire to work more closely with the dietitian. I think there is too much distance between us. They [the dietitians] should have been part of our department. (Registered nurse 1)
Several registered nurses mentioned that nutritional measures, such as the current practice of paper-based dietary recordings, tend to be de-prioritized. Furthermore, although the paper-based dietary recordings have been manually completed, they are often either not entered into the patient record or filled out with insufficient detail. The registered nurses also mentioned that they lack routines for determining the duration of the dietary recordings, and that they struggle to estimate whether the patients have fulfilled their energy and protein requirements based on the recorded intake (Tension for change).
Most of the HCPs were positive that the NUTREAT intervention would fit the current workflow and considered it appropriate that the dietary recordings in the MyFood app would be reported in the electronic patient record. It was also mentioned that the duration of the intervention of 18 weeks might be too short for some patients, as many patients receive tube feeding for quite some time after completion of treatment, and that the intervention is perhaps even more useful when the tube feeding is completed (Compatibility):
Once you’ve removed that tube and are getting used to eating food, that’s when it [the MyFood app] is important. That is the phase we are in now, and which we started a couple of months ago. That’s when it’s important. And I think, especially, if you are a single patient who’s not interested in food, then it might be more necessary. (Spouse 1)
Another potential challenge frequently mentioned by HCPs was poor capacity and little time for new tasks. Therefore, HCPs were concerned that the intervention would lead to extra workload and thus be de-prioritized, despite being positive towards the intervention (Available resources):
It kind of depends how hectic it is from day to day. If one day there are many people asking about support for the app and we really have more than enough with the usual, then it will probably be a lower priority, I would think. And say that, it’s not urgent after all, can you ask again tomorrow? We don’t have the time now. (Registered nurse 3)
Most patients informed that they would have liked to receive reminders prior to the recording periods to increase likelihood of using MyFood on the designated recording days. One patient also suggested that receiving feedback on dietary intake through the MyFood app could potentially enhance motivation to use it. Furthermore, one spouse mentioned that implementing incentives in terms of including a competition or a quiz in the MyFood app might increase usage of the app (Incentive systems).
Most of the participants did not consider the requirement of a smartphone or a tablet for the NUTREAT intervention to be an issue. However, it was mentioned that patients of advanced age or with less resources do not necessarily own a smartphone and therefore must be given the opportunity to borrow a tablet (Available Resources: Materials & equipment).
Implementation process domain
Both HCPs and patients expressed that training and familiarity with the intervention were important prerequisites for being able to carry out the NUTREAT intervention. Furthermore, HCPs expressed a desire for reminders about the ongoing implementation, and feedback on progression (Implementation process: Innovation deliverers, Innovation Recipients):
If we don’t get feedback, don’t see the benefit of it during the first months, then the motivation will probably decrease. (Registered nurse 3)
link





